Your Colonoscopy Experience
 Download PDF
Download PDF
 Download PDF
Download PDF
Your Colonoscopy Experience
We want to ensure that you receive the highest level of healthcare. This means keeping you educated and informed about what is involved in the different stages of your colonoscopy screening procedure. If you have any questions or concerns, please speak with your doctor or medical technician.
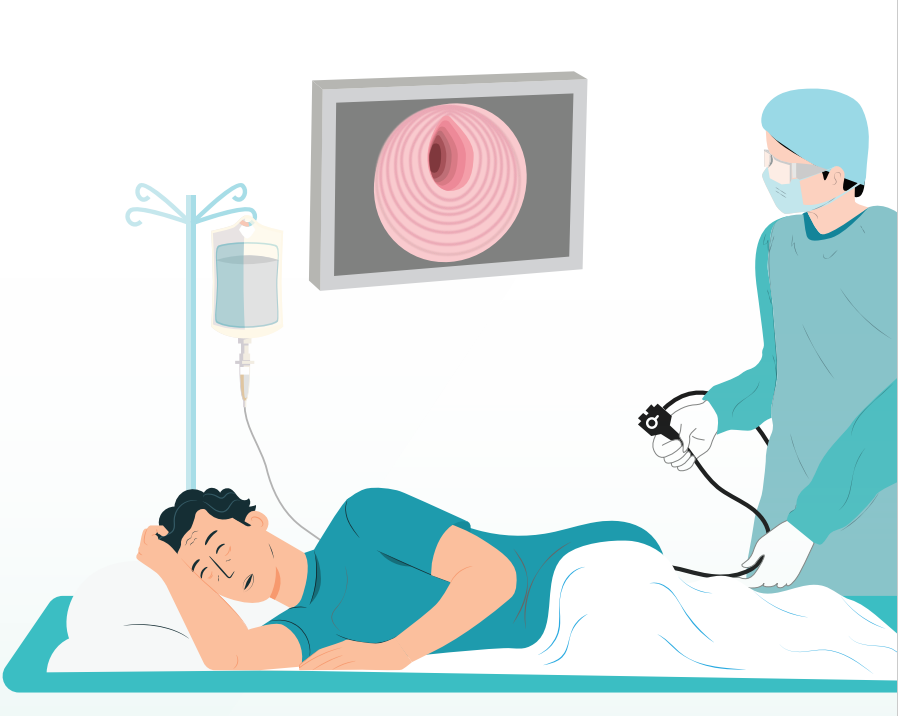
Understanding Colonoscopies
Colonoscopy is a day-care procedure (you return home on the same day you have the procedure) which is done by introducing a colonoscope (a long, flexible tube) through the rectum with a tiny camera that visually examines the inside lining of the colon or large intestine. A colonoscopy can be diagnostic, therapeutic and preventive all at the same time.
Why is a Colonoscopy Done?
During the examination, the doctor looks for changes such as polyps, ulcers, diverticula, irritated tissues and other abnormalities. These can aid in the diagnosis of your symptoms or be used as a screening check if you are over 45 years old. If necessary, polyps or other types of abnormal tissue can be removed through the scope during a colonoscopy. Colonoscopies allow healthcare providers to detect and treat cancer before it develops or spreads and before you have symptoms. Colorectal cancer often doesn’t cause any symptoms until it’s too advanced to be treated effectively.
If your colonoscopy is for screening purposes, your insurance will cover a portion of the cost under your wellness package therefore there will be an out of pocket cost. Please ensure you discuss this with the healthcare facility when booking a date.
If your colonoscopy is for screening purposes, your insurance will cover a portion of the cost under your wellness package therefore there will be an out of pocket cost. Please ensure you discuss this with the healthcare facility when booking a date.
How to Prepare for Your Colonoscopy
Before a colonoscopy, you will need to empty your colon. Any residue/stool may make it difficult to get a good view of your colon and rectum during the exam. To achieve this, you will be asked to:
- Follow a special diet the day before the exam
Typically, you won’t be able to eat solid food the day before the exam. Drinks may be limited to clear liquids — plain water, tea and coffee without milk or cream, broth, and carbonated beverages. Avoid red liquids, such as cranberry juice, which can be mistaken for blood during the colonoscopy. You may be asked to fast after midnight the night before the exam.
- Take a laxative
Your doctor will usually recommend taking a laxative such as MoviPrep or Coloprep, which are available at the Health City Pharmacy. This prep solution, along with plenty of oral liquids, will aid in emptying the bowel.
Special Instructions
- Kindly inform us if you are allergic to any medications or substances. It is important that we know about any history of abdominal surgeries, bleeding disorders, intake of antiplatelets (aspirin, Clopidogrel etc.), anticoagulants (Warfarin, Acitrom, Apixaban, Dabigatran etc.), blood thinners or long-term anti-inflammatory medications.
- Arrange for someone to pick you up from the hospital.
- Don’t drive, make important decisions or go back to work for the rest of the day. You may be advised to
avoid driving for 24 hours following the procedure. - Limit your fibre intake for 2-3 days before the colonoscopy by avoiding salads and leafy vegetables.
The Day Before Your Procedure
(if you are taking MoviPrep)
Take 2 tablets of Bisacodyl 5mg orally in the morning before starting the bowel preparation.
- 12 – 2pm – Lunch: Preferably this should be a liquid meal of soup/juice only. You may have a small quantity of food from the ‘allowed foods’ list. No solid food should be taken after 2 pm.

- 2 – 4pm: Prepare the MoviPrep solution. Each box of MoviPrep has two identical plastic bags, each with two sachets marked sachet A and B. Mix sachet A and sachet B in one litre of water and stir until the powder has completely dissolved. Start drinking the solution slowly and try to finish it over the next two hours. There is no need to rush and a glass (250ml/8+ oz.) every 30 minutes should be sufficient. You are advised to remain in easy reach of a toilet, as the prep should start working within one to two hours.
- If you are not passing stools after four hours of starting the bowel preparation or notice significant abdominal distension/pain/vomiting/any allergic reaction, please seek medical advice. Make sure to drink at least 500ml (about 17 oz.) of clear water/juices/liquids in addition to the 1-litre prep solution.
- 6 – 7pm: Prepare the second 1-litre MoviPrep solution
by mixing the contents of the second plastic bag (sachet
A & B) as before and drink it over the next two hours. Try to drink an additional 500ml (about 17 oz.) of water or clear liquid after this. In most cases, by 11:00 pm your bowels would have emptied, and you may go to sleep.
The Day Before Your Procedure
(if you are taking Coloprep)
Take 2 tablets of Bisacodyl 5mg orally in the morning before starting the bowel preparation.
- 12 – 2pm – Lunch: Preferably this should be a liquid meal of soup/juice only. You may have a small quantity of food from the ‘allowed foods’ list. No solid food should be taken after 2 pm.
- 2 – 4pm: Take the first bottle of Coloprep. Add cool or room temperature water to the bottle until it reaches the neck. Mix well and drink all of the solution over 30 minutes. Afterward, drink at least 500 ml (about 17 oz.) of clear liquids, like water or juice.
- 6 – 7pm: 1 hour after finishing the first bottle, take the second bottle of Coloprep. Add cool or room temperature water to the bottle until it reaches the neck. Mix well and drink all of the solution over 30 minutes. Again, drink at least 500 ml (about 17 oz.) of clear liquids afterward.
The Day of the Procedure
Make sure that you do not eat anything and follow the instructions given by the anaesthetist regarding your routine
medications.
What to Expect During the Procedure
These are the FOUR STEPS you will go through when you come to Health City for a colonoscopy.
STEP 1
You will be admitted 45-60 minutes before your procedure unless otherwise advised by the patient care coordinator. After check-in, a healthcare provider will lead you to a room where you can change into a hospital gown. A nurse will check your vitals such as blood pressure, pulse, oxygen, and place an IV line in your arm to begin delivering sedatives and pain medication to your bloodstream. From there, you will be taken inside the endoscopy room for your procedure.
STEP 2
You will begin the exam lying on your side on the exam table, usually with your knees drawn toward your chest. Once you are comfortably sleeping, the doctor will insert a colonoscope into your rectum. The scope — which is long enough to reach the entire length of your colon — contains a light and a tube (channel) that allows the doctor to pump air, carbon dioxide or water into your colon. This provides a better view of the lining of the colon. The tip of the colonoscope contains a tiny video camera that sends images to an external monitor so that the doctor can study the inside of your colon. The doctor can also insert instruments through the channel to take tissue samples (biopsies) or remove polyps or other areas of abnormal tissue. A colonoscopy typically takes about 30 to 60 minutes.
STEP 3
After the exam, it takes about an hour to begin to recover from the sedative. It’s normal to feel bloated or pass gas for a few hours after the exam, as you clear the air from your colon. Walking may help relieve any discomfort. You may also notice a small amount of blood with your first bowel movement after the exam. Usually this isn’t cause for alarm. Consult your doctor if you continue to pass blood or blood clots or if you have persistent abdominal pain or a fever. While unlikely, this may occur immediately or in the first few days after the procedure, but may be delayed for one or two weeks.
STEP 4
Most colonoscopy results will be shared with you right away. However, if tissue was removed for biopsy, those results will take another few days or weeks. Removing tissue and sending it to a laboratory does not always mean that your gastroenterologist suspects cancer. It could just be a precaution, or they could be looking for something else, like microscopic colitis. They will let you know what they expect to find.
Follow-up Colonoscopies
Your doctor may recommend that you have another colonoscopy:
- In 10 years, if you are at average risk of colon cancer, have no colon cancer risk factors other than age, or have
benign small polyps. - In 1 to 7 years, depending on a variety of factors including the number, size and type of polyps removed; if you have a history of polyps in previous colonoscopy
procedures; if you have certain genetic syndromes; or if you have a family history of colon cancer. Polyps removed during colonoscopy are sent to a laboratory for analysis to determine whether they are cancerous, precancerous or noncancerous. - If residual stool in the colon prevented a complete colonic examination. The schedule for the second procedure will depend on the amount of stool and how much of your colon was seen. A different bowel preparation may also be recommended to ensure that your bowel is completely emptied before the next colonoscopy.
Frequently Asked Questions
Other Patient Pathway Posts
Pulmonary Embolism

What to Expect After a Head Injury

Recovering After A Concussion

How to Care for a Child Who Has Croup

Choking: What You Can Do to Help

Understanding Your Headache & When to Seek Help
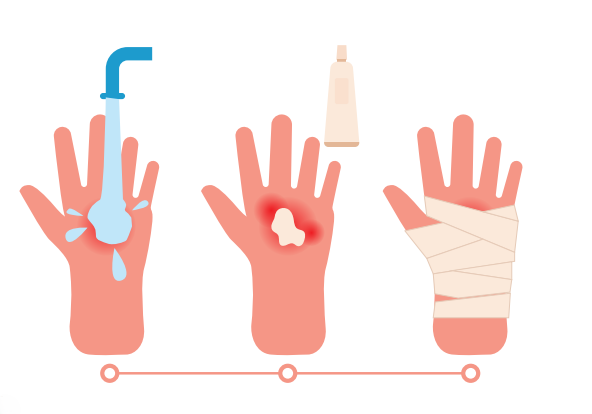
Understanding Burns
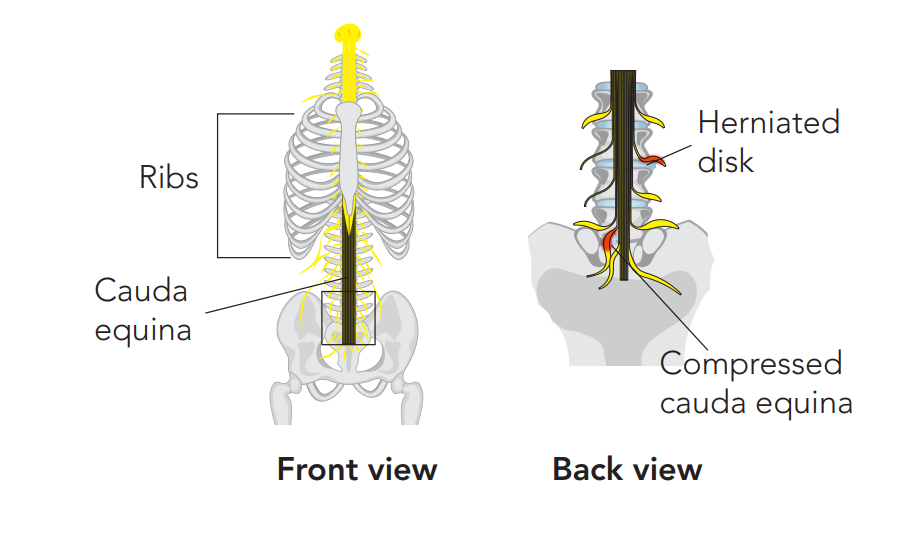
Recognising the Red Flags of Cauda Equina Syndrome
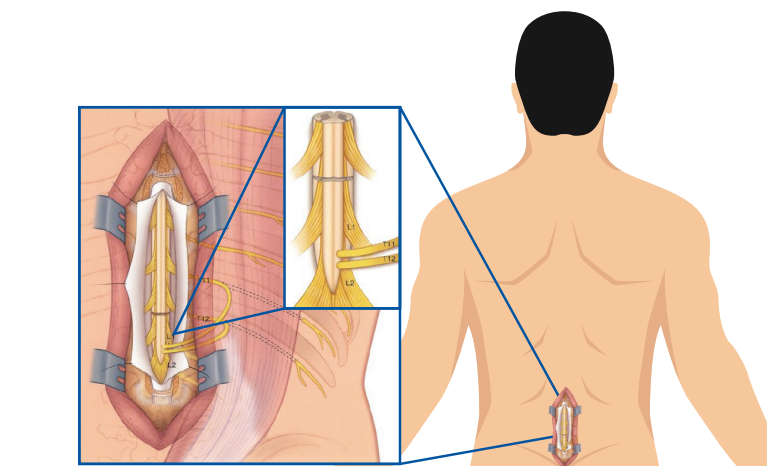
Recovering After Cauda Equina Syndrome

Recovery From Back Pain



